Back Pain – Back Pain During Pregnancy
Fertility, beyond being a reproductive function, includes sacred motherhood; It is a very difficult process where temporary but serious hormonal and emotional peaks are experienced. The expressions on the mother’s face created by the accompanying back and back pain have been a source of inspiration for many artists.
It is a fact that motherhood constitutes the most serious step of transition to womanhood. Some changes, especially in the genitals and characters, give a “mature woman” appearance by slightly regressing. Such a sacred and respected life experience is like an honorable medallion that emerged with this differentiation in female identity.
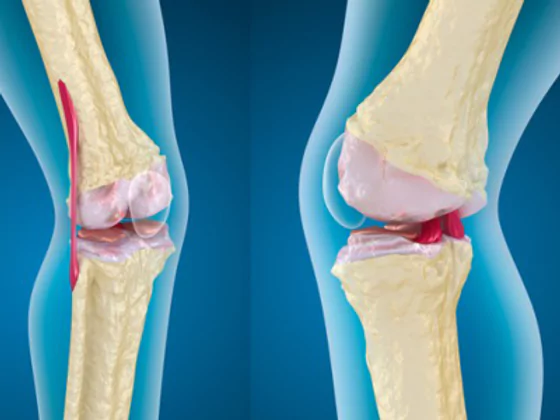
The response of the musculoskeletal system to hormonal fluctuations in pregnancy is not as rapid as the uterus and breast tissue. Skeletal adaptation develops over months and can be described as the defense that responds to destruction in the adaptation process. The bone roof loses strength, its destruction can cause widespread bone pain. The ligament structures that begin to loosen can cause the limits of the joints to be strained during movement and cause injuries. That is why the excessive load on the disc by loosening ligaments of the spine joints causes ruptures in the wall and waist-neck hernias. Spine pain during pregnancy occurs in different stages at different stages. Therefore, different measures will be required at each stage.
Pregnancy is examined in the trimester. However, it would be appropriate to approach pre-pregnancy, pregnancy and puerperium. A mother with a spinal problem before pregnancy should know that her spinal pains will increase and hernias, if any, may progress, and should solve these problems if necessary.
In the first trimester, the weight and mass effect of the baby is negligible, but the hormonal effects are severe enough to change the cycles of the skeletal system. At this stage when placenta formation begins, maternal hormones and fetal hormones compete in the maternal circulatory system.
First of all, we need to know that female hormones have effects that enable skeletal metabolism and bone cycle to work in the direction of construction, increase carrying power and endurance. It is almost usual for estrogen and progesterone to cause complaints characterized by rhythmic cramps and joint pain, even on the moon. These effects are in the direction of construction, but pregnancy hormones suppress this.
Back Pain During Pregnancy – Back Pain During Pregnancy
Pregnancy hormone HCG works in the opposite direction by imitating them, just like the genitals, in the steroid structure we call a kind of gonadotropin. With a slow rise, it begins to suppress this cycle of female hormones and literally takes its place, while bones in the skeletal system prepare a calcium store for destruction, the muscles are forced into a sequence that will work in the direction of pushing. All ligaments tend to increase the elastic tissue structure and loosen. All these hormonal influences are essential for the baby to feed, to provide room for growth in the abdomen, and to progress through the birth canal.
In the second phase, hormonal effects begin to balance. Maternal and infant circulation begin to diverge. As the gestational months increase, the weight of the fetus becomes increasingly vulnerable to daily traumas with asymmetrical loads on the joints due to loose ligaments and the loading of the muscles working in different directions against a moment that will change the body weight center. The second trimester is the transition phase in this respect, the muscles increase their strength against load. In the first two stages, the biggest difficulty in diagnosing the pain of the musculoskeletal system is that the radiological examinations cannot be performed and the drugs that will harm the baby cannot be used.
In the third stage, there is a spine placed in the birth canal in the abdomen that resists an extra 10-15 kg of overload. In this period, if there is aches of muscles that are tired of contraction, joints and ligaments that are injured and healed during pregnancy, pain due to progress in waist and neck hernias occur. When the causes of pain become unbearable, radiological examinations that will cause less harm to the baby are often not accepted by mothers. Drug use may be more appropriate if or not to cross the placental barrier. When our mothers do not agree to take these drugs, it is not possible to relieve the pain.
Labor at the end of pregnancy is a painful process in which the musculoskeletal system is subjected to extraordinary loads. While this miracle is happening, all muscle structures put serious strains on weak and loose bone structures. With a new burden after birth, miraculous hormones (oxytocin, prolactin) that help the milk secretion grow to the rescue of the mother in the postpartum phase. These hormones release growth hormone-equivalent replacement agents (somatomedins). Mothers literally reach the capacity of renewal in a child’s development. This does not occur in normal situations in women who are not mothers, as in men
Breastfeeding mothers suffer less pain after childbirth, and these hormones, which have an endorphin-like effect, relieve pain and also have a miraculous healing function, enter a dramatic production / repair phase within 3-6 weeks. However, the repair process is also painful. These are responsible for the mothers of fatigue, sleepiness, and the tendency to consume sugary foods (puerperal sherbet).
So what should we do so that we can fight back pain?
Spine problems, if any, should be known before pregnancy and their aggravation should be prevented during later pregnancy.
From the first stage of pregnancy, weight training can be performed in addition to exercises such as plates that strengthen the carrier properties of the back and abdominal muscles. However, as we approach the second stage, where the risk of miscarriage will continue to increase, exercises should be performed with plates and isometric movements. Painful situations should be eliminated with cold-hot applications and medical massage, especially without triggering fibromyalgia. Pregnancy is the period of life when ergonomic life is most necessary. Strict compliance with the rules is essential, from the preferred stair step while walking, your seat setting in the vehicle, the way you travel in the bus, the seat at home, to the bench level in the kitchen.
Nutrition, and especially a diet containing calcium, phosphate and plenty of protein, greatly reduces the destruction of the skeletal and muscle structure for the baby’s needs. The mother who is not well nourished is weakened primarily by the body code that nourishes the baby, and it is inevitable that the spine-muscle-originated pains will increase.
If you have a weak body before pregnancy, you should definitely do muscle strengthening in the first months. In the advancing 2nd and 3rd stages, birth preparation groups in pregnancy centers will greatly reduce the pain caused by the skeletal system. Considering that the muscle groups that are tired in the last phase will need more breaks, less repetitive exercises with frequent breaks are preferred.
The needs of the skeleton that heals and regenerates rapidly in the 3-6 week period after pregnancy should be met with rich contents with low calories during pregnancy. The weight gained should be lost, the loads on the spine should be reduced. Pain reduces the transition to some drug treatments in mothers who are not breastfeeding, but I would like to emphasize the presence of natural painkillers for breastfeeding mothers, in this respect, breastfeeding is a great advantage with reducing spinal pain and increasing regeneration.
Pregnancy is the most beautiful period of holy motherhood. Let’s not forget that this period will pass with the least pain and a smiling face, with a healthy diet and regular exercise.